BREAST
AugmentatiON
getting to know YOU
Many implants populate the market, which can be a confusing world to navigate. Patients are often unclear about their target size; we encourage you to bring in photos of your desired look as well as a comparison between your current bra size versus the bra size that you would like to fit into.
As your board certified plastic surgeon, Dr. Lisa Hwang will take the time to thoroughly understand YOU. As the words “bigger,” “big,” and “too big” are widely subjective and open to interpretation, your ideals can get lost in translation, resulting in postoperative dissatisfaction with your chosen size. After getting to know you, Dr. Hwang will guide you with her expertise, providing you with recommendations specific to your body type to help you achieve the look you want!
what bothers you?

size.
Are you unsatisfied with your breast size? Women with small breasts may desire a curvier, more “womanly” silhouette. Some wear padded bras to enhance size and shape, not for support, wishing they could actually fill out their bras of choice. As breast size is determined by genetics, breast augmentation can greatly impact your confidence and boost your quality of life.

deflation.
Women who have undergone significant fluctuations in their breast size, i.e. after pregnancy and/or massive weight loss, may suffer from deflation of their breasts. The skin envelope has stretched, while the breast and fatty tissue within has atrophied. Previously full, voluptuous breasts become small, deflated, and possibly ptotic (sagging), with the nipple hanging low.

shape.
Some women may notice significant asymmetry between the two breasts, while others may have congenital conditions i.e. tuberous breast deformity. Many anatomical landmarks play into breast aesthetics; thus, symmetry may be difficult to achieve. Dr. Lisa Hwang will discuss every nuance with you, so that together, you can decide what is best for you.

Implant options
saline vs. silicone
All implants are made with a silicone shell. The difference lies in the material that fills the implant: saline (saltwater) vs. silicone gel.
Saline implants are FDA-approved for women 18 years and older. They feel slightly firmer and have a higher risk of rippling (visibility). They are more affordable than silicone implants and may be placed with a slightly smaller incision (because implants are filled after insertion). If ruptured, saline implants quickly deflate as the saline becomes absorbed by your body.
Silicone implants are FDA-approved for women 22 years and older. Implants come with varying degrees of silicone gel cohesivity, which range in firmness. Implants with higher cohesivity retain better upper pole fullness. Silicone implants may feel softer, lighter, and more “natural” and have a lower risk of rippling. “Silent rupture” of silicone implants occur because the silicone gel does not get absorbed by the body—it remains within the breast capsule, and can even maintain its shape with increased gel cohesivity. Thus, the FDA recommends routine screening for silicone implant rupture at 3 years after augmentation, and every 2 years thereafter.
smooth vs. textured
Though breast augmentation may seem like a simple procedure, many factors and anatomic landmarks come into play in choosing the right implant for your needs. Many different types of implants have been developed, including smooth vs. textured implants.
Dr. Lisa Hwang generally advocates smooth, round implants and feels that in her hands, they have a superior aesthetic and safe result. In certain situations, textured implants may be beneficial (i.e. they reduce risk of capsular contracture if they must be placed in the subglandular plane). Some women wish for more “natural”-appearing breasts with a gradual slope on top. It is a misconception that only a shaped, textured implant can create a more “natural” look; rather, the selection of appropriate size and profile is what achieves a “natural” transition.
Be aware that textured implants have been associated with Breast Implant Associated Anaplastic Large Cell Lymphoma (BIA-ALCL), a cancer of the immune system, not breast cancer. Though rare and highly treatable, BIA-ALCL currently has a lifetime risk of 1:2,207-1:86,029. As such, the benefits of textured implants don’t outweigh the risks.
size
Implant size is measured in cc's. We understand that these units are difficult to estimate, especially when talking about breast tissue! Dr. Hwang approaches implant sizing by getting to know her patients well; by deeply understanding your aesthetic standards and goals, she applies sound medical judgement (based on your unique anatomy) and a keen aesthetic eye to determine what will make her patients happiest!
Based on her recommendations, you will have the opportunity to try on implant sizers in the office to simulate what that particular implant size may feel like. The day of surgery, Dr. Hwang will be prepared with several implant sizes to make a gametime decision. Intraoperative findings are not always predictable, so it is absolutely critical for you to work with a plastic surgeon who understands you.
profile
Implants are manufactured according to their base width and their projection (profile). As you can guess, implants with higher profiles/projection have greater volume. Generally, patients who aspire for a greater augmentation i.e. 2 bra cup sizes or more, may need implants with higher profile.
Dr. Lisa Hwang will make recommendations based on your physical exam as well as your stated goals. Please do not stress about having to choose the perfect implant dimensions. She will be sure to give you an honest opinion--if your goals are unrealistic, she won't hesitate to decline the procedure. Our goal is to achieve beautiful and long-lasting results.
surgical technique
implant position
Breast implants can be placed in several different locations: subpectoral, subglandular, and dual-plane (combination of both).
Subpectoral implants lie below the pectoralis major muscle, which decreases the risk of capsular contracture. The muscle acts as another layer of coverage for the implant, which is especially important in patients with very little breast tissue to prevent visibility and palpability.
Depending on where the muscle sits relative to the bottom of the breast (aka the inframammary fold), sometimes the origin of the muscle must be released for the implant to settle down into the bottom of the breast, using the Dual-plane technique. Additional release can be performed in patients with mild ptosis (drooping) to achieve a minor lift without performing an actual breast lift (mastopexy).
Subglandular implants lie above the pectoralis major muscle, right below the breast tissue. In this plane, smooth implants have higher risk of capsular contracture than textured implants. Implants have less coverage and may be more prone to rippling (visibility and palpability).


incision
Three different incisions have been described for breast augmentation: inframammary fold, periareolar, and transaxillary.
Inframammary fold (IMF) incisions are superior. They have the lowest risk of capsular contracture. They fade and blend into the breast fold. Residual scars are most easily concealed by clothing. This approach allows the surgeon to have ultimate control over implant placement, which is critical to achieving the best results!
Periareolar incisions hypothetically blend into the border of the areola. However, with poor scarring, the area can become indented and quite obvious, especially if the incision needs to be accessed multiple times i.e. revision surgery. The size of the incision is limited by the size of the areola, which impacts placement of silicone implants. Changes or loss of nipple sensation may occur! This approach requires dissection through glandular breast tissue, resulting in higher risk of capsular contracture.
Transaxillary incisions are desired to avoid leaving any scars on the breasts. However, the armpit also contains apocrine sweat glands, resulting in higher risk of capsular contracture. In addition, both the dissection and placement of the implants are more difficult, with limited visualization and access. The armpit is typically the most frequently exposed area of all. Think about all those tank tops you wear!
SURGERY
Breast augmentation is an outpatient procedure performed at a surgery center under general anesthesia. Primary surgery usually takes about 1.5 hours, including time to undergo anesthesia. During surgery, Dr. Hwang performs rib blocks for local anesthesia. Postoperatively, oral pain medication and muscle relaxants further control your pain. An adult family member or friend should accompany you the day of surgery to take you home and to assist you for the first 24 hours.
Recovery.
Patients can expect some tightness, soreness, swelling, and bruising. Bruising usually resolves within 2 weeks, while swelling may take up to 3-4 weeks to resolve. After surgery, you will be placed in a supportive bra, which you should keep on for the first 2-3 weeks (except for showers). You can remove all dressings and shower the day after surgery. I encourage you to move your arms around slowly (i.e. out to the sides and over your head) to preserve the range of motion of your shoulders and back.
Avoid any heavy lifting over 10 pounds and avoid pushing anything (i.e. heavy doors, shopping carts, etc.). Patients with desk jobs can return to work within one week, but more strenuous physical activity should be avoided for 6 weeks. Initially, implants are generally larger and high-riding with swelling, but they will gradually settle into the bottom of the breast within 6 weeks. Please be patient!
Risks & Complications.
Risks of breast augmentation include bleeding, infection, capsular contracture, implant rupture, implant malposition, asymmetry, BIA-ALCL with textured implants, and possible need for future revision surgery.
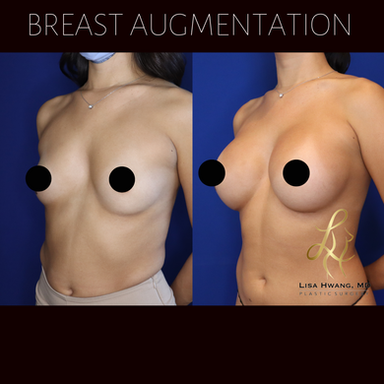
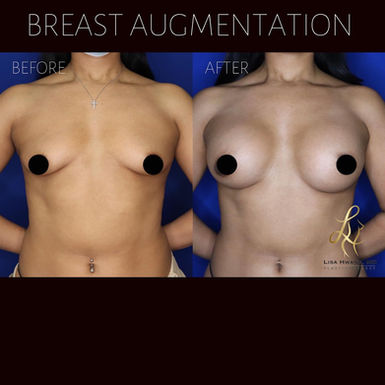
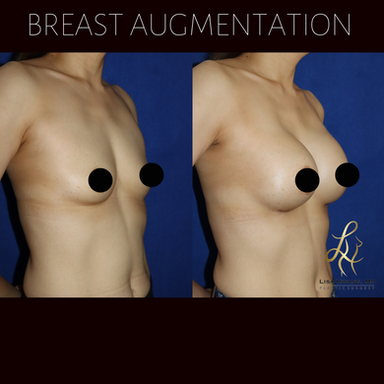
Results
Videos
Breast Augmentation
Breast Augmentation


Breast Augmentation

Mommy Makeover

Breast Augmentation Operating Room (OR) Video *WARNING - contains GRAPHIC images
REVIEWS
"Dr. Hwang is absolutely amazing! She did an outstanding job on my breast augmentation/revision. It was not an easy case, I had a lot of scarring and capsular contracture. The end result truly speaks to her talent as a surgeon, I could not be happier!" — Patient Review on Yelp
"Honestly, words cannot describe how happy I am with my breast augmentation experience with Dr. Hwang. She's so kind and understanding on top of catering to what my goals and vision are for the outcome I had in mind. I literally cannot get over how my post-op breast surgery came out and it's only been day one! I have already received so many compliments from my friends that knew about the surgery with comments like: "it sits perfect and natural" and "it's very proportionate." I'll come back to update on my progression photos as recovery and healing time goes by!" — Patient Review on Yelp
"I had breast augmentation done by Dr Hwang. It's only been 4 weeks since my procedure and I couldn't be happier with my results! My breasts look so so natural and in proportion to my body. My main goal was to have cleavage and fill out my bathing suits and that has definitely been delivered!! As for my scars, wow Dr Hwang is an artist!! I was so nervous going in for my first consultation but I was immediately put at ease by Dr Hwang, she answered all my questions and concerns and I knew she was the perfect Surgeon for me. The whole procedure from consultation to recovery has been a breeze. Dr Hwang is also my go to for Botox. Like I said before, she's an artist! My only regret is not finding her sooner. :)" — Patient Review on Yelp
FAQS
How do I choose my desired implant size?
With more than a decade of surgical expertise, Dr. Lisa Hwang takes a personalized, science-based approach to implant selection. During your consultation, she performs a thorough physical exam and precise measurements of your unique body frame to determine the range of implant sizes and profiles that will look most natural and harmonious on you. You will then try on sizers to simulate and confirm which sizes you like.
While online forums often suggest “bigger is better,” the truth is that ideal sizing is far more nuanced than a number on a box. Here, we guide you step-by-step through the process, explaining implant shape, profile, cohesivity, and volume. We size scientifically—not by guesswork—to ensure that your ultimate implant choice fits your anatomy, matches your vision, and ages beautifully for a timeless result that feels entirely your own.
Do breast implants cause breast cancer?
No. Breast implants neither cause nor increase your chances of breast cancer. They also do not impact or delay the detection of breast cancer. There are, however, two other types of cancer to be aware of: Breast Implant Associated-Anaplastic Large Cell Lymphoma (BIA-ALCL) and Squamous Cell Carcinoma (SCC), which will be explained below.
We advise that you adhere to standard guidelines for breast cancer screening with mammograms, as recommended by your primary care provider (PCP). If you’re undergoing breast surgery, we require an up-to-date mammogram for women over the age of 40. For women with significant family history or personal breast cancer history, mammograms may be recommended earlier.
What is BIA-ALCL?
Textured (not smooth) breast implants have been associated with Breast Implant Associated Anaplastic Large Cell Lymphoma (BIA-ALCL), a cancer of the immune system, not of the breast. Though rare and highly treatable, BIA-ALCL currently has a lifetime risk of 1:2,207-1:86,029.
The risk varies among different implant manufacturers, as they all use differing manufacturing techniques. In July 2019, Allergan announced a voluntary worldwide withdrawal of unused BIOCELL® textured breast implants (and tissue expanders), as they had been found to have an increased incidence of BIA-ALCL compared to their counterparts. However, the risk was still considered to be “low;” hence, the FDA does not recommend that all patients with BIOCELL® implants undergo surgery to remove them.
Presenting symptoms of BIA-ALCL include delayed unilateral breast enlargement, pain, asymmetry, skin rash, night sweats, or large fluid collection developing more than one year after augmentation, averaging 8 to 10 years. Patients who develop any of these signs should notify their plastic surgeon immediately for evaluation and imaging.
Diagnosis is confirmed with fluid aspiration and cytology/flow cytometry for CD 30+ large anaplastic T-cell lymphocytes. PET-CT is performed following a positive diagnosis. Treatment involves removing the implant along with complete (bilateral) capsular resection. The majority of cases are cured with good prognosis; however, rare patients may present with more advanced disease, possibly requiring radiotherapy and chemotherapy.
BIA-ALCL is being closely monitored and researched. The FDA recommends that any suspected or confirmed cases of BIA-ALCL be reported to the PROFILE registry, the MAUDE database and the device manufacturer.
Do breast implants impact mammogram screening for breast cancer?
Mammograms are an effective and recommended way to screen for breast cancer in women with breast implants. Breast implants do not delay diagnosis of breast cancer. However, saline and silicone implants can obscure adjacent breast tissue, especially in the subglandular position (above the muscle). Implants placed in the subpectoral position (under the muscle) are much less likely to interfere with the interpretation of the mammogram. Additional Eklund views are performed to better evaluate the breast tissue.
Women with breast implants should continue to undergo breast cancer screening with a mammogram as recommended by their primary care physician. Recommendations differ among various governing agencies, but annual mammograms should generally start between the ages of 40-45, unless you have increased risk of breast cancer (i.e. family history), in which case you may consider getting mammograms earlier.
If you have breast implants, make sure to do the following:
1. Find a facility that sees many women with breast implants
2. Make sure to inform the staff at your appointment that you have breast implants
3. The facility should obtain special mammogram views (Eklund)
4. Perform monthly self-exams. If you note changes in your breast, please inform your doctor promptly.
Do breast implants cause Breast Implant Illness?
Breast Implant Illness (BII) has been termed to refer to a constellation of vague symptoms, including chronic fatigue, joint/muscle pain, memory/concentration problems, skin rashes, anxiety, depression, headache, hair loss, gastrointestinal problems, etc. Patients have reported these symptoms after breast augmentation, either immediately or years later.
BII is not currently recognized as an official medical diagnosis. It is poorly understood, as there are no diagnostic tests or diagnostic criteria. No concrete lab or blood tests can confirm association or causation of breast implants with these symptoms. Some suggest that BII is related to autoimmune and connective tissue disorders, such as lupus, rheumatoid arthritis, and scleroderma. However, only some patients with BII actually get diagnosed with a specific autoimmune or connective tissue disorder.
Existing medical literature does not show a definite association or causation between breast implants and autoimmune/connective tissue diseases. Nevertheless, Dr. Lisa Hwang acknowledges that these symptoms may develop in select individuals. Her approach is to first rule out other potential causes. If the symptoms persist, breast implant removal can be considered with the understanding that the symptoms may not necessarily resolve following surgery.
How long will my breast implants last? Will I need another surgery?
Breast implants will last as long as you are happy with them and aren’t suffering any complications. There is no absolute shelf-life at the end of which implants must be switched.
Generally, there is a 10% chance of implant rupture at 10 years, as well as a risk of developing capsular contracture. With the increased cohesivity of the newest generations of silicone implants, the silicone gel contained within the silicone shell remains cohesive and no longer extravasates into the implant pocket. Dr. Lisa Hwang utilizes surgical techniques that have shown to minimize risk of capsular contracture, such as making the incision under the breast in the inframammary fold, placing the implant under the pectoralis muscle (or partially under the muscle in dual plane), and “no touch technique’ using a Keller funnel.
Everyone may succumb to the natural sequelae of aging and life changes i.e. pregnancy and weight gain/loss, which may cause a waterfall deformity, or drooping of the breast. If you are not having any of these problems, your implant may potentially last upwards of 20 years.
What credentials does Dr. Lisa Hwang hold?
Dr. Lisa Hwang, MD, FACS is a board-certified plastic surgeon specializing in aesthetic surgery. She is certified by the American Board of Plastic Surgery (ABPS) and has completed extensive training, including full residencies in both general surgery and plastic surgery, followed by an aesthetic surgery fellowship endorsed by the American Society for Aesthetic Plastic Surgery (ASAPS).
Dr. Hwang is an active member of several esteemed professional societies, including ASAPS, the American Society of Plastic Surgeons (ASPS), the California Society of Plastic Surgeons (CSPS, and the American College of Surgeons (ACS). Her practice reflects a commitment to surgical precision, artistic vision, and compassionate, personalized care.
What does a Breast Augmentation cost?
Costs can vary based on your individual goals. Reach out to us with the details of what you’re considering, and we’ll provide a ballpark estimate.